
In our Own Words: UK doctors talking about our own mental health
- by Louise Freeman & Angelika Luehrs
- •
- 20 May, 2019
- •
Doctors' Support Network (DSN) co-chairs, Dr Louise Freeman and Dr Angelika Luehrs, presented at the 2019 European Association for Physician Health conference in Oslo about speaking openly about our own mental health as doctors and how this has changed since DSN was founded in 1996.

Doctors' Support Network background
Dr Louise Freeman first explained how DSN had started and developed over the last twenty years.
'The Doctors’ Support Network is a confidential peer support network for UK based doctors and medical students with concerns about their mental health.
Early years The organisation was founded in 1996. GP Dr Soames Michelson had published an advert in the British Medical Journal asking if there were any other doctors with mental health problems and Dr Lizzie Miller, the first female trainee neurosurgeon in the UK, was one of the thirty doctors who replied. The group approached leading UK medical organisations for support. These included the General Medical Council, the British Medical Association and the Royal College of Psychiatrists. They were told ‘I think you’ll find that you’re the only ones’! At this stage, there were only two peer support organisations in the UK – both for doctors with addiction - and little formal physician health. Early group activities included face to face meetings and a newsletter.
The network started an online, confidential support forum in 2001. Membership of the forum was restricted to doctor members of DSN. The forum allowed doctors to informally support each other while navigating being unwell with mental illness. Adding medical students to the forum was considered at one point and rejected by a majority of members partly due to worries around confidentiality. At this time, the committee only published their first names on the website and did not have their photographs either – photos were only added in 2013.
DSN Stigma Survey In 2014, DSN surveyed our members about their experiences of stigma - find out more here. A typical example of the type of experience recorded was ‘I experienced two years of pretty florid physical symptoms of anxiety/ depression (weight loss, early morning wakening, panic attacks) before attending my GP for help, mainly because I really wanted to be able to cope, and everyone around me seemed to be coping fine. I didn't want to admit to failing.’
In the UK in general, very few doctors spoke openly about having had mental ill health due to a combination of felt and enacted stigma. The stigma of mental ill health is well known to lead to delays in seeking treatment as well as poor responses from colleagues and others to mental ill health.
Unfortunately, my own experience of becoming sick while working as a consultant in emergency medicine involved experiencing much felt and enacted stigma including being told that a colleague had 'always thought that I was a mental health problem waiting to happen!'. I joined DSN in 2011 and became vice chair in 2012 and I've been co-chair with Angelika since 2018. I have gained so much from volunteering with DSN and connecting with other medics with similar experiences as I got better having definitely felt as if I was the only one while I lost my job.'
Louise then handed over to Angelika to talk about her experience of working as a consultant psychiatrist while having a diagnosis of Bipolar Affective Disorder.
It’s ok not to be ok and the art of speaking up.
Dr Angelika Luehrs said:
'It is ok not to be ok was the title of a piece on my Trust’s website about my experience of being a doctor with mental illness. It is ok to be a doctor and suffer from a mental illness and it should be ok but not always is as yet, to be open about it. Therefore, awareness raising is for me an essential activity. Raising awareness of course doesn’t mean wearing a sticker stating ‘I suffer from bipolar Illness’ – it would be counterproductive and irritate people more than being helpful. There is a time and place for awareness raising. But that’s not always easy and we (DSN) thought it would be interesting to reflect on the choice of activities to raise awareness and the impact of being open about having a mental illness as a doctor. The following points are my own experience and considerations although I have discussed them with others and found that people in similar situations and also friends/family and professionals mostly agree. All of the examples are my own as well.
About me I work as a consultant psychiatrist in Wiltshire, UK since 2010 and as a specialist advisor for complex mental health cases with the NHS GP Health service since 2017. I suffer from Bipolar Affective Disorder and was diagnosed in 2004 during my training. This was somewhat unexpected and caused significant disruption to my training. I was initially hesitant to get help and scared whether or not I would be able to continue with my career. I had never heard of a doctor with bipolar illness. I wasn’t really worried about medication, side effects, prognosis – all the questions my patients ask me. Of course, my illness caused major disruption to me training but overall the key issues have been medication and significant side effects. For example, I have photosensitivity as a side effect of one of my mood stabilisers which on occasions causes more problems than my illness. It is amazing how much emphasis we put on our role as doctor.
I wondered if there were any other medics out there and was signposted to DSN. I have been involved with the organisation since 2005. I realised that I am not the only doctor with mental illness and that there is more stigma attached than I had realised. In addition, I heard the negative experiences of colleagues and found that I have been very lucky with the support I received from professionals and my Trust as an employer. I decided that I was in a good position to speak up, personally and due to my support. Speaking up is a great thing to do but needs to be carefully considered. Once it is out there you can’t take it back.
So I would like to share with you some of the insights I’ve gained over the last fourteen years.
Factors to consider:
Support system This includes for me friends, family and professionals – people I would contact when I become mentally unwell. They need to be aware of any activity such as interviews etc and support it. My psychiatrist has been crucial with his advice about how and when to speak up and when not to.
Own mental health It is important to be mentally reasonably stable (that is of course very individual) when undertaking these activities. Raising awareness brings up memories, emotions and therefore almost always leaves me feeling somewhat vulnerable and raw. It makes me more self-conscious and worried about what people think for a while until this settles again.
It is also important to have considered all factors prior to deciding about awareness raising activity such as your frame of mind, support, possible consequences and what to say. For example, being elated in mood is not the time to agree to an interview and go ahead with it. This leads to another key point – how much do you feel comfortable to disclose: diagnosis? Related problems? Symptoms? How much detail of symptoms? I for example don’t mind talking about my diagnosis, symptoms in general but not in detail. Why not? Because I don’t think it is important and I wouldn’t feel comfortable about it.
The other important factors for me are around work:
Employer I have always included my employer in any decisions around awareness raising on national and international level. This usually includes a conversation with my line manager or, for example for the television show, with my medical directorate and communication department. I was keen to ensure that the Trust is supportive of my activity and would be happy to intervene in case of any problems. Also I had to make sure that the Trust is happy to be in the press/social media. If my Trust hadn't agreed and been supportive, I wouldn’t have done some of the activities. I have been very lucky with the support and responses from my Trust. They have been very supportive and are actively promoting our activities on their social media and local radio.
Medical and non-medical colleagues This is a very interesting aspect as you would think that it is not a major issue as the whole idea is about speaking up and raising awareness. However it is a lot easier to disclose my diagnosis and challenges to strangers rather than locally. Some of the most nerve-racking moments were a talk to my team, the Trust Board and also knowing that my team was watching the television show on which I appeared. How would my junior doctor feel about his consultant with a mental illness? How would I feel in the next Leadership Forum knowing that all senior managers know? These are the questions you need to feel confident to answer prior to agreeing to any awareness raising activity.
And last but certainly not least:
My patients Last but not least, I need to maintain a professional therapeutic relationship with my patients. There is a lot of talk about disclosing own experience of illness (physical and mental) and how this impacts on the patient-doctor relationship. There clearly are advantages to it such as own experience and, in some professionals' and patients' opinion, better understanding. I don’t think that the understanding is ‘better’ as such but rather different. Every illness and the perception of it is individual depending on factors such as symptoms, nature of illness, culture, personality, up-bringing and many more. The way I experience depression will be different to others but my overall understanding of it will differ from somebody who has never suffered from depression at all. It doesn’t make it necessarily better though.
What to do if a patient asks about my mental illness I have of course been faced with the situation of a patient reading about my mental illness as a result of looking me up online. Therefore you do need to prepare for this and what you would say in the threatened scenario of somebody challenging you ‘how do I know you are not unwell’ or simply asking you for more details?
Managing information I also consider how my patients and families/carers might feel reading for example in the newspaper about their consultant having a mental illness. I personally don’t think that that’s a good way of finding out and therefore would not consent to a piece about me in the local paper. This is very different to something posted on Twitter by my Trust, DSN or another professional organisation. This is also somewhat protective as it implies that they are aware and don’t have an issue with it.
There are clear positives though which for me outweigh the potential challenges by far:
- There is an element of safety
in disclosing one’s illness rather than keeping it a secret and being worried it might cause problems. It makes it easier for an employer and I am thinking in particular about local colleagues to act and to support if they are aware of a problem in the first place for example on-calls.
- In general, of course the more we talk about having a mental illness the ‘safer’ it gets until having a mental illness as a doctor turns into something acceptable,
something that needs managing but nothing else.
- There is positive feedback
which makes it worth-while from colleagues and other doctors with mental health problems.
At medical school I was confident that I would never choose psychiatry as a subject. I was going to do emergency medicine or general practice (GP) and be a ‘proper ‘doctor’. I then had to do psychiatry as part of a GP rotation and loved it. Not because it helped me to understand myself – I actually thought I knew myself pretty well but clearly didn’t as well as I had thought! Apart from realising that I find psychiatry exciting and interesting as a field of medicine I also found patients and staff inspiring and have met some fantastic human beings. I never saw mental illness as anything other than something we can learn to manage and control. It would have never occurred to me to perceive anyone I met as weak and unable to do the things they would like to do simply as a result of having a mental illness. Obviously, there are limitations externally and as a result of illness, but this is not the place to discuss these.
The greater good And finally, for me the key point is being part of something good, something important and bigger. As I said at the beginning, I was very lucky with the support I received both from professionals and employer feeding into and strengthen this attitude. I was therefore open about having a mental illness from the beginning and developed the drive to take this further. '

AndMe anti stigma campaign
'A turning point for DSN as an organisation was our participation in the Royal College of Veterinary Surgeon’s cross professional Medical Minds Matter event in 2015. I represented DSN at this event and spoke about my own experience of low mood and depression after a bereavement reaction. The reason that I spoke at the event was because no vets would speak openly about their own mental health. I realised that doctors seemed to have more of a problem with our own mental health than vets, pharmacists or dentists and I thought that this should change but we then had to work out how to enable people to do this as safely as possible.
So in 2017, we started our AndMe campaign with the Royal College of Veterinary Surgeons' Mind Matters initiative in order to create a group of senior health professionals with lived experience of mental ill health who could show that a psychiatric diagnosis had not meant the end of their career. An AndMe volunteer writes their own text and supplies a photo for online use. We are very careful in selection of our volunteers to make sure that people are sufficiently well and in a robust career situation. For example, we ask our volunteers to check with their employers / work partners as well as their close family to make sure that those around a volunteer are positive about their proposed involvement in the campaign.
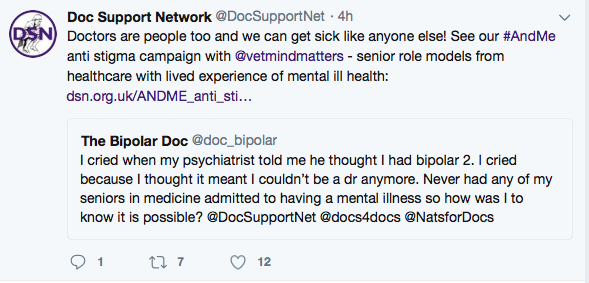
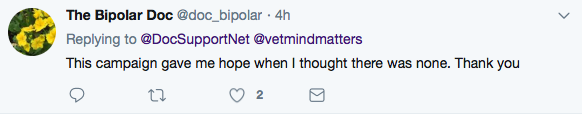
There have been some amazing responses including this from a trainee paediatrician who tweets as bipolar doc:
Around the AndMe campaign, DSN also collaborated with a German group 'Selbst betroffene Profis' in presenting a symposium at the 2017 World Psychiatry Association Congress in Berlin about the value of peer support for health professionals (while owning our own history of mental ill health).
And in the last year, DSN has appeared on BBC television’s Victoria Derbyshire programme in a film about physician suicide and provided senior doctor volunteers willing to openly talk about their mental health for BBC radio discussions.
So from not having our family names or photographs on the DSN website, we have graduated to frequently contributing to broadcast articles about physician health under our own names - in fact it might seem as if we now never shut up about it!
Key messages for doctors considering talking openly about their mental ill health include
- Is it the right time for YOU?- health / career / personal life considerations?
- What are you trying to say? Generalisable positive messages are good!
- Talking about your own health experience has a cost to you - it's not like doing a normal presentation at work
- Recognise and acknowledge that other medics' experience may be quite different to your own

Doctors' Support Network
DSN facilitates informal peer support via an online, confidential, anonymous forum, face to face meetings and an AGM and conference. The photo above is from our most recent conference in Edinburgh in 2018. DSN is free to join with a suggested donation.
Find out more on our main website here

DSN Mailing List
Please complete the form below if you would like to receive occasional updates about DSN and UK physician health by email (AND you are not intending to JOIN DSN - if you are joining DSN, you will be added to our members' mailing list). Mailing list contacts CANNOT access our anonymous, confidential, members only Support Forum - for Full or Student members only.
How to JOIN DSN as a Full, Student or Associate member - click here.
Updates can include invitations to take part in physician health surveys by other individuals or organisations. We will not use your contact details for anything else unless you say we can. You can find out more about how we store and use your data and what your rights are in our privacy policy.
A DSN update will be a formatted email (using Sendinblue ) with an 'unsubscribe' option.
DSN mailing list
We will add your email address to our mailing list.
Please try again later
Follow us

Disclaimer
All opinions expressed on this website are those of the individual authors and do not necessarily reflect an official position of DSN. DSN cannot accept responsibility for any actions taken as a result of content of the website. Links to other organisations are provided for information only and are not a recommendation. In particular, you may want to check about confidentiality when contacting other organisations.








