Sample quote
'It took me a very long time to get over feeling ashamed and profoundly guilty for my illness (depression). And in the earliest stages it took me a long time to accept what I knew logically the diagnosis was because of these feelings.'
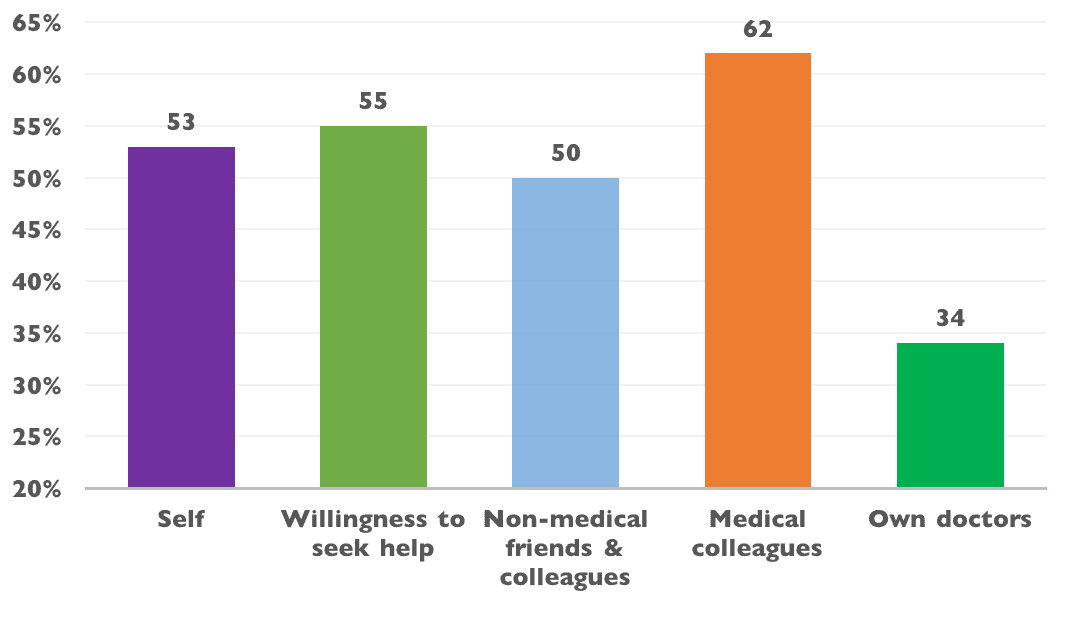
Stigma affecting willingness to seek help70 respondents (55%) reported that stigma had affected their willingness to seek help, and that this had delayed accessing support.
Sample quote
'I experienced two years of pretty florid physical symptoms of anxiety / depression (weight loss, early morning wakening, panic attacks) before attending my GP for help, mainly because I really wanted to be able to cope, and everyone around me seemed to be coping fine. I didn't want to admit to failing.'
Stigma affecting interactions with non-medical colleagues and friends64 doctors (50%) reported difficult interactions with non-medical colleagues. Thematic analysis revealed 'denial' and 'shunning' as common issues.
Sample quote
'Whilst an in-patient suffering an episode of depression I was allocated a new CPN (Community Psychiatric Nurse). I was visited on the ward by this CPN and the CMHT (Community Mental Health Team) manager. They told me that as I had previously worked in psychiatry I should know better than to allow myself to become unwell, and that I should know the tightness of reserve in the NHS, so should not be wasting peoples' time or taking up a valuable bed space.'